So here we are again. For many years I have taken notes at
this particular meeting and have made them available to any EMS provider or
manager willing to take the time to read them. There is a lot written below, so
I am going to get straight to the disclaimer and not add any more reading time.
Please remember that these are my raw notes with only one pass at spelling, grammar,
and content correction. Take them as they are. I have tried to relay the speakers’
intent and key points in each summation, but this is never a perfect process.
Enjoy!
Eagles 2025 – Hollywood, Florida – Seminole Hard Rock
Hotel/Casino
Day One
Pepe – Intro – Discusses history of the Eagles. FDMs are the
final decision makers on what happens in EMS. The medical directors represented
at Eagles cover nearly one third of the American population. Thanks everyone
for being here.
Antevy – Intro – Welcomes everyone to southern Florida. Next
year the conference will be at the Broward convention center to the east of the
current location.
Augustine – Intro – It has been a challenging five years. A
lot of different challenges in serving our communities from a lot of different
directions. Thanks to Paul Pepe for keeping this show on schedule.
Goodloe – ACEP welcome to Eagles. Pepe discusses an 1891 art
image of a physician watching over a patient at a home bedside with Goodloe.
“That’s what we do, we go there, watch, and deliver care.”
Caruso – Welcomes everyone on behalf of the fire community
in the area. “Soaring to New Heights” is the motto of Eagles this year.

Colwell – The Pentagon Papers: Five Most Important
Publications of the Past Year – Could not get it down to five papers so he is
doing five topics. Trauma resuscitation – TXA prehospital, significant survival
benefit with no increase in complications. There was a dose specific
improvement in mortality with the 2 gram dosage. 1 gram does not work very
well. Weak evidence for use in brain injury. Strong evidence for prehospital
administration in hemorrhagic trauma. TXA and blood combined with prevention of
hypothermia, early hemorrhage control and limited fluid resuscitation save
lives. ACLS in trauma - CPR in trauma patients?
Literature set is growing on ACLS use in trauma. Should we be doing it?
Epi in trauma patients? Does not appear to improve outcomes. Prehospital vital
signs - vital signs are extremely
important for comparison with emergency department vital signs in predictive
value. Abnormal vital signs in the field predict serious injuries. The article
was mainly regarding children. Traumatic Pneumothorax – 42% of prehospital
needle decompressions did not have a pneumothorax. 30-92% did not reach the pleural
space. C-collars – C-collars analyzed in children. Very few have injuries. C-collars
torture patients. Not sure if the c-collar provides any benefit. Using it a lot
with a lot of evidence that we do not need this tool. No studies showing
benefit. There is proof of harm. Ditch the c-collar whenever we can.
Weston/Miramontes – Why Do EMS Systems Need to Become More
Attentive, More Involved, and More Assertive in Managing Perinatal/Postpartum
Emergencies? 160/110 for only 15 minutes can cause end organ damage from 20
weeks before to 6 weeks postpartum. Severe hypertension is fairly common in
this group. If you don’t look for it you may not find it. Very few will have
hypertension as the chief complaint. We are missing severe, damaging,
hypertension in our prehospital cases. Pathophysiology of preeclampsia: a disorder
of widespread endothelial malfunction and vasospasm. If the baby does not get
what it needs, it gets pissed off and releases hormones that affect the mother.
Six weeks postpartum is a time frame that is a big deal for maternal deaths.
Preeclampsia can happen postpartum. SBP DBP ENTER FROM SLIDE. Use Mag Sulfate
in the midrange and Mag Sulfate and antihypertensives in the high range.
Labetalol, Hydralazine, and Nifedipine are suggested as choices. Nifedipine is used
orally in some BLS systems. Postpartum hemorrhage is a big deal. Oxytocin is
still recommended, and the studies show it works. Patients should go to
appropriate facilities.
Mackey – What are “OB Deserts” in Maternal Healthcare – OB
Destinations – MIH Roles: An OB desert is defined as a county that has no
hospitals providing OB care, no birth centers, no OB/GYN and no midwives. 35%
of US counties have zero OB care. 217 maternity wards have been closed since
2011. 29% of critical access rural
hospitals are on the verge of immediate closure. Reasons? There is a shortage
of OB/GYN physicians. OB is not financially viable for most hospitals. High
cost of malpractice insurance. We need community birthing centers. We also need
to attract OB/GYN physicians through better insurance reimbursement and loan
forgiveness. Support at expand use of midwives and MIH Community Paramedics.
Colwell – How Should We Deal with precipitous Deliveries and
Other Acute OB Emergencies: Normal deliveries have very little participation.
Do normal procedures, dry baby and keep warm. Biggest issues? Breech 4%,
Shoulder Dystocia 3%, and prolapsed cord. Describes a twin breech vaginal
delivery. Complete, Footing and Frank are types of breech deliveries. Do not
pull. Hands off until umbilicus is delivered. Once umbilicus is delivered, we
can assist using the Mauriceau Maneuver. Shoulder Dystocia. Look for the turtle
sign. Several maneuvers available that each take 30 seconds. If one does not
work move to the next. McRoberts maneuver, Wood’s Corkscrew maneuver, and the
Gaskin maneuver can all be used. Consider episiotomy. Umbilical Cord Prolapse:
Must be decompressed. Insert fingers to keep baby off the cord. Think about
these before they happen. We must be able to intervene.
Bradley – How Should We Navigate Sudden 911 Responses to
Birthing centers? When a birthing center calls 911 things are not going well.
The wheels are coming off the bus when they call. These are high liability risk
with adverse outcomes possible. Interactions with high stress staff can be
stressful. What is the licensing/oversight of the facility? Cases currently
across the US. Work collaboratively with the birthing center. Play nice in the
sandbox and kill them with kindness. Know when to escalate reporting of issues.
There is an AABC toolkit available to these facilities that discusses working
with EMS. Document everything on these calls. Be detailed and factual. Avoid
stating your opinions.
Maternal Missions Panel –
Ramos/Weston/Miramontes/Mackey/Colwell/Bradley – Diana Ramos is the Surgeon
General for California. Discusses fetal mortality in the US. Describes a case
with a patient with severe symptomology and the fact that no one asked if she
was pregnant. Follow up on maternal patients is an issue. There may be a lack
of resources available to the patient for postpartum follow up as well. Miramontes
states that he has 11 lines of care going within his MIH program. Postpartum is
one of them. We don’t know the social determinants of health that affect each
patient as we do not see their house and living conditions in the ER, but the
paramedics do know it and see it. We must remove the hard guardrails on what
EMS can do. We need to think about our roles as healthcare in the US is not in
the greatest shape. How can we reform ourselves to be what our communities
need. Consider pregnancy in any woman of childbearing age. Have guidelines for
caring for these patients. Hard to transport these patients out of rural areas
as it may take a crucial coverage ambulance out of its 911 role locally. Establishing
maternal levels of care nationally is in progress. Texas does this already.
Discussion on how MIH-CP is being funded in several communities.
Schaefer/Nayles/Holcomb/Antevy/Bank - Prehospital
Transfusion State of the Art – How Far Have We Come? What are the Current
Hurdles? What are the Disparities, Unclarities, and the New Verities in the
World of EMS Transfusions? Why is Plasma the New Headliner? How’s Our
TBI-Plasma Protocol Playing Out? Are There Other Uses for Prehospital Plasma
like Burns/Sepsis? 120 ground services ding blood and blood products last year
and 254 doing so this year. If you cannot get LTOWB use Plasma. There are too
many people dying to wait for the availability of LTOWB. Blood suppliers are
concerned about proliferation of need. See the Prehospital Blood Transfusion
Coalition for advocacy. Agencies can join this coalition. Still some barriers
in some states regarding administration of blood to pediatrics. Blood not just
needed for trauma. Can be used for AV fistula issues. Some systems approach
need of blood as close to 50% medical related causes. Not for adults only. Case
study presented on pediatric blood loss from tonsillectomy. Most systems carry
blood on supervisor vehicles rather than the ambulance. TXA and Plasma may be
more available to be able to get onto every unit. TXA in TBI has a slight risk
of seizures but provides good outcomes. Early TXA treatment is better. Ditch
the salt water, plasma is better. Plasma does not increase brain edema. Studies
are starting but the data is already compelling. Brain vessels are unique. They
are designed to not have leakage. TBI causes leakage. Use of saline increases
brain vessel leakage. Multicenter RCT has begun. Plasma may be the next
frontier for TBI, Trauma, Sepsis, Burns, Warfarin reversal, and Ace-I induced
Angioedema. Child who was in case study above brought on stage. Multiple cases
of good outcomes in giving whole blood to pediatrics. Antevy says you need to
push back if your system does not allow blood administration to pediatrics. Will
discuss the role of Calcium in a later session.
Bank/O’Byrne/Vitberg/Roach/lowe/Banerjee/Jenkins/Holcomb/Schaefer/Marino/Calhoun/Goodloe/Miramontes/Kazan/Lawner/Ahndebach/Pease/Valenzuela
– What are the Other Considerations and Adjuncts Du Jour: Calcium in the field?
When do you use it? Calcium deficiency has been raising its ugly head as we
further discuss blood transfusions. Associated with higher mentality. There is
a sweet spot when discussing calcium levels. Calcium Chloride is better than
Calcium Gluconate in this application. Supports a study on use of Calcium in
the absence of lab values. “Just because a number is low does not mean we need
to fix the number.” Seems to be a bit of a split on thinking on whether to
utilize Calcium in the field without values. One speaker notes that paramedics
are dealing with multiple priorities in this scenario without having to worry
about getting Calcium onboarded. Walking Blood Bank concept and process
discussed. One physician describes his experiences in war zones being
introduced to hospital workers giving their own blood for patients. The Walking
Blood Bank concept is very localized but akin to establishing a reliable donor
pool. In fact, reliable donors are essential to a walking blood bank. A case
study presented on a rural mass casualty event where significant blood
resources were sent using a regional system. The plan is to use a walking blood
bank as the next stage as needs escalate. DC is giving a unit of blood on average
every 30.2 hours. Whole blood is dropping the DC trauma index and dropping the
number of actual homicides (by improving the rate of trauma saves). DC uses a
blood dashboard that shows the location of supervisors with blood and time left
on each blood product till expiration. Discussion on IM TXA. Decreases time to
TXA administration dramatically if giving it IM. Does shock index correlate to
mortality? Not in the case of these treatments. The treatments on the front end
(such as blood started during crush syndrome) defy the mortality of the trauma
index. Whole blood and TXA is very effective in reducing mortality. Discussion
on aerosolized chitosan. It is OTC. The spray comes out cool. Needs to be at
least 6” away from wound due to pressure at nozzle. Avoid deployment in
confined spaces. Washes out with water. Creates a hemostatic matrix on surface
exposed. Revisited the AutoTQ concept. Great strides made in the product. Chicago
and Amazon are both deploying the AutoTQ for use. It is an automated,
push-button tourniquet that self-tightens. IV fluid shortages have been
occurring again. No money in making IV fluids. Low margins and very high
regulatory burden in manufacture. There is no back up or redundancy in fluid
supply. There is a machine that will now manufacture normal saline on site at
the hospital. This device breaks down the choke points of shipping and or
remote areas. It will produce LR and D5W as well.
Calhoun - What is Cincinnati Considering in terms of
Prehospital Blood Infusion? Are we bloody well right? Is blood infusion
beneficial with low transport times? What is the cost/Benefit? How well does
combat data apply to civilian EMS? How does blood apply to non-traumatic
hemorrhage? What are the drivers in the decision making? Plasma is $70 while
whole blood is $475. What can be gained by one over the other. Only 13%-14% of
donations can become LTOWB for infusion. What are we saying? Do the research.
Do YOUR research? Make sure your programs help your patients.
Marino – Why are Big Easy Trauma Receiving Red Blood Cells
Versus Whole Blood? Blood in the Big Easy. New Orleans has 70 Blood trained
paramedics. Giving about 100 units of PRBC a year. Using Calcium and TXA as
well. Time matters. They are starting two units of PRBCs in less than five
minutes. Why not whole blood? WB is more expensive and had no redistribution
route. Packed RBCs could be rotated with supplier. Has impacted homicide rates
simply with PRBC treatment keeping more victims alive. Fewer trauma patients
required intubation with use of PRBCs. Why do it with short transport times?
For every minute blood is delayed, mortality is increased by 11%. It is faster
to start blood products in the field than it is for those in the hospital.
Katz/Kuhlman – Isn’t it Time to Formally Designate Receiving
Centers of Excellence for Out-Of-Hospital-Cardiac-Arrest? We have specialty
centers for trauma and stroke and to a certain extent STEMI, but what about for
cardiac arrest resuscitation? We could easily get better data and practice this
way. Why does it matter? There are greater than 350,000 patients annually with
less than a 10% survival rate. High volume of a patient type to a given
facility increases expertise and survival. This is not for every hospital, but
expertise would improve outcomes. Currently the center of excellence exists as
a voluntary certificate of attestation but need to be escalated to an external
review for accreditation. Primary status must have a termination of
resuscitation protocol. Must participate in CARES. Comprehensive must have 24/7
CVICU coverage. Going to transporting only to a resuscitation center moved one
service from a save rate of 8.3% to 16.6%. This needs development of national
standards. It should be desirable to everyone to use this concept. Hospitals
that see the same thing over and over again get really good at what they do.
Cheskes/Miramontes /Jui– DSED/VC and the Warranty – Is
DSED/VC ready for prime time? ERC came out recommending VC over DSED. DSED
doubles survival rate. DSED is superior to normal defib in all aspects. VC is
better than normal in all criteria of measurement except for neuro intact
discharge. Neuro intact discharge was only improved by double sequential
defibrillation. His system (Toronto) uses AP pad placement for normal
defibrillation. Names Stryker as the only one putting up a barrier to
proliferation of DSED (common knowledge) due to warranty issues with
defibrillator damage. Only simultaneous double defib has shown to damage a
defibrillator. Another study coming soon on DSED. San Antonio is doing DSED
after 1st shock. Two vectors, two shocks, to time frames. First
shock lowers impedance. If DSED fails then ECMO may be the next option. Is
Amiodarone being given too late in the arrest? In many cases, Amiodarone is
being given at 20-22 minutes after onset of cardiac arrest. There comes a point
where you are shocking a heart that cannot convert. There is a critical window
for giving antiarrhythmics. Our goal should be Amiodarone withing 8 minutes of
ALS arrival. Slight advantage with Amiodarone over Lidocaine. Improvement in
survival (including neuro intact) if Amiodarone is give early. The earlier the
Amiodarone is given, the better the chance of positive outcomes. Studies from
Korea, Australia, and the US. Antevy states that he has removed Epi from the VF
protocol in his systems. Two studies show that Amiodarone is ineffective when
given via IO.
Dunne/Sanko/Bronsky – Evergreen Programs to Establish,
Enhance, and Continue to Focus on the Various Elements of Heart Safe
Communities: The communicate has to recognize arrests to be able to get to
paramedic resuscitation efforts. Designation as a HeartSafe Community is a big
deal as it builds a foundation to enhance the patient prior to EMS arrival. Public
education, prevention, training and incident recognition is crucial.
Administered by the Citizens CPR Foundation. Data collection includes CARES and
defib registry. You have to commit to training 15% of your population every
year. Used hands only CPR outreach. The city council in Detroit has purchased
50 AEDs for community placement. They improved T-CPR provision. Leverage school
police for AED placement. Emergency Action Plans in public buildings must be
updated. Heat map arrests to show high likelihood areas. The take home message
is that this can be done. Includes survivor support initiatives as well. El
Paso has the four-minute community roadmap. What barriers are there to AED
usage? Are they in the right places. We know that early CPR and early AED
increases survival by almost 50% depending on rhythm. Do a time analysis on
when arrests occur. Response time analysis on cardiac arrests only. Analyze age
of arrest patients. The majority of arrests worked in the US have EMS arrival
after five minutes. AEDs are getting smaller and getting smarter tech. History
of arrest can be downloaded from use of a QR code. Trying to assure that CPR
and AEDs are within four minutes of potential use.
Margolis – Preparing for Chemical Warfare in EMS Response
and Training: If you were a bad guy, what chemical agent would you want? Fast
and effective, rapid onset and lethal/incapacitating effects. Points out nerve
agents and asphyxiants and opioids (where there are also antidotes available).
How do we deliver the right care at the right time in a CBRN environment?
MARCHE2 – Mask up, Antidotes, Rapid Spot Decon, Countermeasures (antidotes in
the hot zone and medical management), Hypothermia mitigation, Extrication. Life
threatening hemorrhage can be controlled in the rapid spot decon phase.
Discussion on organophosphate. Watch out for bronchospasm, bradyarrythmia and
the things that will kill you quickly. How much Atropine do we give? Enough.
Keep giving it until you do not need it. 2-PAM Chloride needs to be used as
well to separate the toxin from its ability to affect the nervous system. Cyanide
poisoning? The cell cannot utilize oxygen. Treated by Cyanokit. Assure that we
use airway control, advanced monitoring, and oxygenate these poisonings.
Marino – Recent Truck Attacks in NOLA: Showed video of NOLA
truck attack. 14 killed and dozens injured. Continuity of command maintained.
Police department was providing care. Triage tags were not used. Markers were
used on patient faces instead. Worked very well. They realized much after
arrival the entire operation was in the hot zone. There were bombs present that
they were unaware of at the time. Majority of patients were red or dead. 71
patients total. Only 9 yellow and 8 green. EMS transported 29 patients in 95
minutes. 14 deaths and 57 injuries eventually attributed to the incident. Started
thinking about what to do for employees in the incident next.
Asaeda/Antevy/Feldman/Goodloe – Receiving Facilities are
de-facilitating across North America: Should 911 agencies provide interfacility
transports? If so, when? Rising EMS call volumes are happening. Often running
out of ambulances to dispatch. Hospital closures. Increasing regionalization of
care. When in doubt, hospitals are now calling 911. Most common patients for
this are trauma, STEMI and stroke. OB, ortho peds and psych are the next most
common. Pennsylvania law says they cannot fail to respond based upon keeping
ambulances available for other runs. Are emergency departments shifting EMTALA
responsibility to EMS? The Philadelphia legal department now reviewing this
issue to see what they will do. LA traditionally did not use 911 for transfer
work. In early 2000s they started doing trauma center transfers, then it became
STEMIs, then the “patient dying in front of you” exception. 69 hospitals in LA
county. They drew the line at strokes and started to say no. Hyperspecializing
of hospitals is adding to the transfer problem. Perinatal services are becoming
more rare as departments close. LA drew a line. They will only do transfers out
of the ED. No CCT (no vents or IV pumps). Be a facilitator and not an enabler.
Make what you will do clear. Advocate for proper reimbursement ( speaker adds
that hospitals need to pay for these transfers). Montgomery County Maryland
uses the term “emergency transfer.” Call volumes are up as well. If call
volumes are up, they issue an emergency transfer stand down to assure unit
availability. Is it ethical to use 911 resources? 911 patients in the field do
not have any other help. Transfers are not the primary mission of EMS. “The
transfer patient cohort is in the presence of doctors.” Maryland has taken the
stand that emergency transfers should be rare, the hospital should provide
adequate personnel, and the agency has to have the availability to do it. This
should be done only after all other resources have been attempted. You cannot
commandeer an ambulance going available at your facility. Under EMTALA with a
laboring patient, stabilizing equals delivery. An occasional ask is also
different from a habitual expectation. Some systems may be set up for both
missions. Ontario provider requires the hospital to provide personnel in the
ambulance for transfers. From a coding perspective, they have found that the
IFT patients are most often sicker than the 911 patients.

Antevy/Asaeda/Feldman/Kupas/Dominguez/Gindling – Panel
Discussion on a Number of Short Term Fixes – that May Also Increase Risk: One
NY hospital gave a two-year warning on closing which gave time for planning.
Type of hospital closing matters. A smaller NY emergency room and three bed
hospital closed by putting a flyer on the door with no warning. Closure
increases load on other hospitals and increases EMS wall time, which
increases
response time due to less availability. Brevard County Florida had a hospital
close that covered a needed area. 46-day warning. At the first meeting venting
was allowed, after that only solutions. Legislators are looking at rules to
prevent short notice hospital closures. Same things are happening in Ontario as
well. What is happening with finances in the hospitals has a dramatic effect on
what happens in EMS. Community hospitals survive on a 1 to 2% profit margin.
Wall delays at hospitals negatively impact EMS provider budget and ability to
fund wages and availability. OKC/Tulsa spent 2.4 million dollars in lost
availability due to wall time in one year. You have to speak to hospitals in
the currency language. See the Rand Report from EMPI and ACEP. See the ABC-ED
Act of 2025 (bipartisan supported bill to address hospital boarding). 
Asaeda/Mackey/ Lawner/Satty/Swanson/Bronsky - Not Bypassing
the Closest Hospitals: NYC is taking to closest appropriate. Not allowing
patient choice in destinations. Continuity of care does not equate to medical
necessity. The California system is asking four questions instead of the normal
three for 911. They are asking police, fire, EMS, or mental health. If the
caller says mental health, they are shunted to 988 rather than a response.
Day Two
Paul Pepe welcomes everyone to the last day of Eagles 2025.
Gaither – How Does a Fire-based Special Ops Team Help with
Aerospace Recovery Missions? Discusses current space missions to and from the
ISS and Space X. Talks about Boeing Starliner. When something like Starliner
lands on the ground it becomes your jurisdiction. Starliner uses a 300-mile
target for landing. It is just another special operations response. Physical
hazards: it has a static charge, has hazardous materials onboard (hydrazine).
Decon is with water. Albuterol is used if wheezing. Seizures possible. Same as
any other hazmat, use hot zone concept and approach from upwind. Set up decon.
Level B gear for decon. Specific space related illnesses like volume depletion
and space vertigo. How do you respond to a spacecraft in your backyard? Do what
you do every day.
Simpson/Kazan – What’s the Experience with an Imbedded
Pharmacist in Our EMS System? There was a growing number of questions to the
pharmacist regarding EMS pharmacology within this service. A pharmacist can be
fully imbedded in the medical direction team. Pharmacists can answer questions
like: why do your protocols use this dose of that drug? Can answer drug storage
problems like light exposure and temperature. Their pharmacist took EVOC. The
pharmacist has been oriented at a level to deeply understand the field and EMS.
The pharmacist has also co-authored scientific articles regarding medications
in EMS.
Katz/Cheskes/Banjeree/Antevy – Progress and Hurdles with Abx
for Sepsis: Katz: Mortality rates in hospital is 20-25%. 30-60% of all sepsis
patients arrive at the hospital via EMS. Time and antibiotics are the key to
survival in sepsis. Discusses sepsis protocol and screening tools for a sepsis
alert. They also use shock index as a component of their sepsis screen. The
studied use of Ceftriaxone. 183 patients received the antibiotic. Tachypnea was
most common presenting system followed by altered mental status. Zero allergic
reactions. Mortality in this patient population was 4% when compared to
pre-study. Blood cultures were impacted. Contamination of cultures went down 4%
as well. Blood cultures drawn at hospital after administration. It takes an
hour from patient arriving at ED to get antibiotics started. This is much
slower than getting it started in the ambulance. Narrow the scope down to
obvious sepsis patients and you won’t be overtreating and get the med to those
who need it most. Antevy: His system gave antibiotics to 1308 patients last
year. Large study coming out of Toronto soon that will change the EMS focus to
insure sepsis treatment: PITSTOP Trial. A study that “should be burned” is the
one out of the Netherlands on antibiotics in ambulances. Problem with
Netherlands study is that the patient population was not very ill. Target of
Toronto study is a 5% reduction in mortality. Antevy is converting to Cefipime
from Rocephin. They are including peds except for newborns. Physicians on stage
gave their experiences as well which were similar. Hospital resistance and griping
was a common factor. Antevy: “They keep telling me that I make too many
protocol changes and they want me to stop.” Do what you need to do.
Simpson – Experience with Buprenorphine: Opioid death rate
was really high. There is an opportunity to make a difference. Keys to
implementation were cost effective (tablets) realistic training at less than an
hour, and goes on every truck just like any other paramedic medication. No
precipitated withdrawal has been noted. Over 70% patient improvement. Now over
200 administrations and have seen a larger number of patients seek treatment.
This was in Hennepin County.
Lowe/Satty – Various Perspectives and Various Initiatives
for Follow-ups: Ohio: This is a harm reduction program labeled as outreach. The
day after to 48 hours is best contact time. Need multiple contacts. Resource
intensive but pays off. Live conversations are better than texting. Team is
composed of a paramedic and a dressed down police officer in a fire department
vehicle. They can also delay court proceedings but not reduce charges. 743
people followed up on. 304 linked to treatment. It took 3 or more attempts to
get them to link to treatment 52% of the time. New Jersey: OD response team.
Goal is to shorten the time between EMS contact and the patient receiving
formal treatment. Mapped their overdoses. Community workers work with the
paramedic on the team. The referral to care is integrated into the EPCR. The
consent to follow-up is built into the normal consent signature for the run.
428 referred with 53 placed into treatment programs. Just added a nurse
practitioner to the team. Includes providing transportation to care. Expanding
Buprenorphine to all units.
Mechem - From Xylazine to Medetomidine, additives to
Fentanyl: Xylazine is known as “tranq” and is added to Fentanyl. Now seeing
Medetomidine. Both are veterinary sedatives. 91% require ICU admission, 24%
require intubation. Treatment requires opioids and sedatives. Medetomidine is
not widely regulated. It is here to stay. Profound respiratory depression and
bradycardia. Can be treated but there is not antidote.
Weston - What is the Benefit of Public Facing Data and
Community Education in the Opioid Crisis? EMS has the richest data set.
Naloxone is prevalent. They publish overdose trends. Also showing data of mixed
overdoses. They also heat map the overdoses as to where they occur in the
community. What is the value of public facing data? Targeting where to provide
efforts is a key benefit. Partner with academic entities to leverage their data
management people.
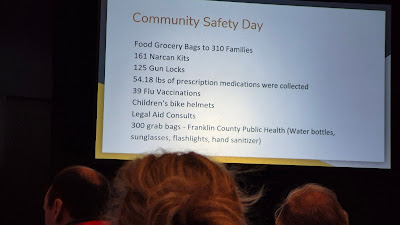
Lowe - How Can We Leverage Drug Take Back Day for Community
Outreach? Can we do Narcan training and other community education such as bike
courses, helmet usage and vaccinations? What about food distribution? Used a
lot of kids’ activities. It may be easier for you to come to drug take back day
if there are other reasons to come. Increased participation in the event. How
do you manage the volume of attendees? They did this as a drive through event.
Mechem – How Should EMS Manage the Accelerating Number of
Persons Requiring Wheelchairs? Surgeons are recommending more amputations due
to non-compliance in wound care. Replacing a wheelchair is hard with insurance
companies if one is lost. Wheelchairs tend to get stolen if left behind. If the patient has no wheelchair with them it
increases costs for hospitals and delays transport home. Wheelchair transport
by EMS is now allowed if it can be secured and not interfere with care or
vehicle operation. Wheelchair must be covered as most are soiled. Wheelchair
vans are also used for empty wheelchair transportation.
Jui – Is Naloxone Infusion Helpful in Out-of-Hospital
Cardiac Arrest? This talk documents the obvious, but there is not a lot of data
that it improves outcomes. Existing AHA data
was indeterminant. Portland has run an observational study. There was a high
peak on overdoses last year. Naloxone has no effect on anything other than
opioids. How could this improve OOHCA outcomes? Opioid OD can lead to cardiac
arrest. Believed to be an effect on pseudo-PEA. Restores respiratory drive-in
opioid OD. Reversal of bradycardia and hypotension. Theoretical belief that
Naloxone may improve CNS protection in cardiac arrest. Inhibits Microglia
Activation which stops the inflammatory response. Early naloxone was given IM
or IN Naloxone prior to IV or IO Naloxone. Included LE administered Naloxone.
Looked at data by rhythm as well. Marked increase in ROSC and discharge neuro
intact in the PEA population (not Asystole). Supported by the Dillon 2024
article on the same subject. EMS administered Naloxone was associated with
clinically significant improvements in ROSC and survival to hospital discharge.
Antevy states that he supports Naloxone in all arrests if there is any
possibility of opioid OD.
Persse – All BLS Ambulances? Can That Really Work in a Major
City? This is a presentation out of Houston. What is the goal? To save lives.
What does that take? Bleeding control, airway, and defibrillation. We also need
good customer service and the ability to handle complex medical calls. Where do
paramedics fit? They are not needed for the top three reasons we respond.
Sometimes you need the extra skill set but it is not the first need. They are
mainly needed for complex medical calls due to higher level of training and
critical thinking skills honed by experience. 71% of EMS encounters result in
transport. A maximum of 20% transported need ALS skills. 49% of communities are
lengthening response time goals. 28% have moved to tiered systems. 23% have
transitioned away from dual paramedic response. Transitioning to ALS
non-transport decreased paramedic response time by 19.1%. This is significant.
Also experienced a 3-minute response to cardiac arrest cases. This caused a 30%
increase in patients found in VF. And this reduced the paramedic attrition rate
(due to increased job satisfaction). My Note: I have pushed this as a system
model for years. Simply better on the paramedic and better patient care. This
also stops having to pressure people to go to paramedic school and creates a
more desirable career option for the paramedic. Sometimes there is a belief
that this is a degradation of care when in fact it provides better care. This
took educating local politicians and the community. FDNY Medical Director
states that they are primarily a BLS system. FDNY is in the middle of trying to
go to this as well but is having issues finding enough EMTs to backfill the
ambulances.
Simpson – POCUS, Thousands of Patients Later – So What
Surprised Us? Practice on your non-critical patients so that you get good at
it. You can always upgrade acuity based on findings. You can never downgrade
acuity based on findings. They use a fixed charging dock inside the patient
compartment for storage. POCUS can be used to guide pericardiocentesis. 100%
feedback is given on every ultrasound taken. All paramedics are POCUS trained
in their system. P3 level paramedics are trained in more advanced POCUS exams.
About 10% of the time the cardiac/lung exams lead to a change in treatment.
Over 6000 POCUS exams have been performed. It is an additional way to confirm
ET tube placement.
Stone – Mastering Some of the Limitations of Ultrasound
Application in the Field: If just starting, pick a few goals like looking for
blood flow in PEA, for ROSC, and for TOR. Defining futility in PEA is difficult
but POCUS can make this easier. Acquisition of skills is fairly easy, and it
sticks. Needs to be done by all to keep from offering disparate services 24/7.
Can also be used to assess carotid artery flow. Flow has been present in 26% of
PEA cases which makes it easier to make a TOR decision and not stop on a
patient with actual flow. TOR is indicated for true futility situations.
Dunne – Is Transesophageal Echocardiography a Viable Field
Tool (for several reasons)? Just starting a pilot program in Detroit. High
quality CPR is the key to survival. A study from 2007 regarding where hands
placed on the chest in the standard CPR position, 80% were not over the left
ventricle. You have to stop compressions to do ultrasound. You do not have to
stop CPR to do Transesophageal Echocardiography. The probe that connects to the
device is disposable. It connects to any tablet wirelessly. Provides very good
images even while rolling in transport. You can see every compression from the
angle provided in the imaging. The pilot program will last for the next 12-16
months. More next year.
Banerjee – What Does Polk County Use for PEA Cases? Bundling
for PEA. Survival to discharge in PEA is less than 5%. Narrow QRS vs. wide QRS,
if wide QRS it is more likely medical in origin. They do airway, manage ETCO2,
and give Narcan. Then Epi, Bicarb, 1gm calcium, D10W, then a saline bolus. In
the US there has been a 1400% increase in opioid associated cardiac arrest.
Bundling improves ROSC and survival to discharge. They are seeing 18% survival
to discharge.
Rice – A Strategy for Identifying Pre-Arrest States and
Avoiding CPR: EMS witnessed arrests are almost always proceeded by warning
signs. In 2019, 9.4% of their arrests had been seen by EMS in the previous 48
hours. Vital signs in those cases appeared to be predictive. Implemented a
crashing patient bundle for patients with SBP less than 70. Used fluids an push
dose pressors. Once implemented the number of EMS witnessed arrests dropped
significantly. The most common excuse given for not using pressors was “we were
only five minutes away from the hospital.” They explained how much time is
saved by doing the on scene care. More impactful to treat early. Pull up push
dose Epi while starting fluid bolus. Expectation is that push dose pressor is
pulled up and ready before entering ambulance.
Miller – Can We Use EMS Resuscitation to Enhance Viable
Organ Donation: Speaker is from Dallas. Case study presented. 17-year-old
hanging. It was a very chaotic scene. Incredible resuscitation attempt. Got
ROSC. Post ROSC care and survival to admission. Brain death confirmed. CPC 5.
Arrest management was perfect but was not recognized due to it not being a neuro-intact
survival case. The family chose to donate six organs which saved several lives.
What is the role of EMS? In most of these cases, we must have ROSC to be an
organ donation candidate. Dallas Fire-Rescue accounted for 11% of all donors
and organs transplanted in that locale. The EMS crew was recognized for their
role in providing a viable case for organ donations. Cultivate a relationship
with organ procurement and find a way to recognize crews who play a role in
assuring a viable patient for donation through excellent management of care.
Holley/Goodloe/Bachista – Brief Updates on Neuroprotective
CPR: Where are we at with neuroprotective CPR? Very few places are doing heads
up CPR. Edmond, Oklahoma experience. Several years ago, they implemented one
device. ROSC was not impacted significantly. But 100% of those witnessed
arrests who had ROSC after a shockable rhythm, survived to hospital discharge.
Data has been consistent for over three to four years. Using an active
compression decompression device and ICD as well. Memphis: They are seeing
almost all CPC1 survivals, or they do not survive. Gave case study of a
64-year-old prominent cardiologist who collapsed on a golf course who survived
with neuroprotective CPR. Neuroprotective CPR has outperformed CARES data for
the last five years. The study will be out soon.
Antevy – How Well are we Preparing EMS and Emergency
Departments for Childhood Cases? “Every battle is won before it is fought.” –
Sun Tzu. Put the kids with the adults. Out of 378 code 3 transports there were
over 400 incidents or near misses. Mentions the national EMS pediatric
assessment. You have to have a person passionate about pediatrics to take on
the gap analysis and improve. An agenda of improvement needs to be created to
drive the improvement. Showed video of EMS personnel training ED staff in pediatric
cardiac arrest drills. Leadership includes driving practice. We must practice
to drive performance. You determine when to leave the scene on a pediatric
arrest before you arrive on scene. You must stay on scene to drive care that
results in survival.
Antevy – Should We Now Be Applying CPAP in Kids? There are
several conditions where peds can benefit from CPAP. Cincinnati has a pediatric
CPAP protocol. Essentially the mask must be correct. Flow Max and Go Pap are
two that work well for kids. There are adapters that must be used for it to
work. https://bit.ly/m/Peter-Antevy-MD?r=qr
Kuhlman – What are the Lessons Learned from the Nuclear
Navy: High Reliability Healthcare is a buzzword. 98,000 deaths a year in the US
due to medical error turned out to be a way too conservative number. The think
tanks looked to airlines and other industries as examples in how to reduce errors.
There are errors of omission and errors of commission. The principles of high
reliability do not work well at the bedside. When trying to learn from
spectacular disasters organizations turn to the nuclear navy. The nuclear navy
has a 75-year history without a nuclear accident. The engineering part is the
easy part. The hard part is changing the culture. The navy was following a
culture of status quo (follow orders, do what you are told, don’t ask
questions, never challenge superiors, not forthcoming, situational). The
Pillars: Higher level of understanding, Integrity of the individual and the
organization, formality of procedure and communication, question when something
is not right, and back each other up. Uncommon persistence is needed to achieve
this level of change in a culture.
Weston – Why is Continuing Medical Education So Essential?
Standard education schedule + clear expectations and repercussions for
non-completion = Da 1 assigned, Day 30 due, Day 31 overdue reminder, Day 50
notice to provider and chief, Day 60 suspended.
Gilmore – Should We Continually Assess Skills, Performance,
and Behavior? How many have set through the same old education time and time
again? Did we really reinforce or educate anything doing that? The education
agenda for the future kicked the competence can down the road. It is being
created now at the national level. Multi-faceted agenda steering committee.
What is continued competency? There is now a definition. The current system is
too complex. There is no consideration of on-the-job performance. No
consideration of changes in technology. Not a systems approach. The concept of
hours needs to be replaced with credits. If you have already proven competence,
how do we recognize that in the secret sauce? Can we get credits for number of
skills performed? The patient benefits from us being competent. The medical
director and the agency must have skin in the game as well. Of course, you as a
caregiver have skin in the game as well. Can this be automated through EPCR
vendors? How long should a recertification period be? We don’t know. New
providers need a shorter recertification cycle while more experienced could
have a longer period. We need to stop kicking this can down the road and fix
it.
Holley – How Should We Educate Our Educators? We stretch
instructors too thin. We need to train them to be better instructors.
Instructors need better orientation. Needs to be a dedicated individual who
oversees the entire educational curriculum development. The mentoring process
needs to be continuous. There needs to also be study skills workshops for
students along with tutoring, mentoring, and access to learning resources. Must
eliminate deficit thinking. Students need wraparound services (transportation,
broken phones, schedule help... we will take care of you). There should be an
instructional advisory board.
Cozzi – Anatomically Exploring Enhancements in Knowledge and
Performance of Responders: Benefits for the caregiver to use cadaver labs for
initial and ongoing training. Demonstrates anatomical proficiency, enhances
procedural competence, and integrates anatomy with critical decision making.
Provides hands on experience, provides more accurate injury identification, and
better patient safety by using cadavers. Directly reduces errors. The brick
wall is the cost. $6,500 + shipping to get a fresh frozen cadaver to Chicago.
Being used by the Chicago Fire Department.
Holley – What is the Value of Non-traditional Satellite
Training Centers for EMS Continuing Education? A closed navy training facility
was acquired and started reaching out to various types of organizations to see
if it could be used for training. Assessed on site housing, wifi, simulation
space, classrooms, AV systems, etc... space for drone training, search and
rescue site, and more. Needed to be multi-disciplinary. Were the agencies able
to contribute instructors, share equipment, provide financing, etc... What did
we do? Created what was needed and the appropriate spaces for all needs. The
property provided is now neutral ground for many disciplines to use.
Jui/Marty – What are Upcoming Infectious Disease Threats EMS
Should Know? H5N1 Avian Influenza in the US. Focus on the D1.1 Variant.
Seasonal flu is also no joke. Most pandemics are from a form of avian
influenza. Then it needs to cross to humans and have human to human
transmission. H5N1 is a hybrid virus. 50% mortality rate. 70 reported cases in
the US. This is driving up egg costs. The risk to general public is currently
low unless working in the bird/egg industry. First detected in the US in 2024.
D1.1 has an enhanced binding to human type receptors. H5N1 crosses into cats,
cattle, wild birds, poultry, and rats. Primary worry is transmission to humans.
We depend on flu shots, and antivirals. Measles is back and it can kill you.
Before widespread vaccinations, Measles caused 2.6 million deaths a year. There
is a 14 day incubation period. Measles is still in the top 10 killers of
children in the world. Measles spreads easily and quickly. This was eliminated
in the Americas and now it is back. This is a bad thing. Measles vaccine is
$1.14. Three deaths have occurred in the US. Discussion transmission, like
viruses and case definitions. Measles rash starts in 2-4 days (speaker knows we
are being told 4 days, but it can start in 2 days). It can cause convulsions
and neuro deficits. Give fluids and anti-fever medications. There is no
antiviral for Measles.
Feldman – What Happens When the Chemical Threat is in the
Hospital? CBRNE response to hospitals. Discussed case where fumes from phenol
formaldehyde exposed patient made to the hospital and required evacuation of
the ED and ORs had to be closed as it entered the ventilation system. Another
case was covered regarding Malathion (organophosphate) making it into the
hospital on a transported patient. Some hospitals plan to call fire and EMS to
handle patients inside the hospitals. Poison Control sometimes has a long hold
time.
Augustine/Dunne/Calhoun – What’s in My Fireground Toolkit? Case
studies regarding CN antidote usage. When synthetics burn they create toxic
byproducts. CO and CN are issues that cause death in smoke inhalation. No one
wants to see soot or burns inside the airway and mouth. CO must be monitored
with firefighters on the fire scene. Clothing can off gas after leaving scene.
If CO and fire are present CN is likely as well. Look for weak, dizzy,
diaphoresis, headache, AMS, dysrhythmia, chest pain, seizures and cardiac
arrest are all signs of CN poisoning. Anyone on the fire scene can be exposed.
PPE is essential to prevention. Every headache does not need the antidote. The
antidote is a limited resource both on scene and at the hospital. Do not rush
fire scene injuries, fight that impulse and truly take care of the patient.
Pedi dosing is becoming more common. In one case the smoke went up an elevator
shaft and caused smoke inhalation on the top floors.

heat stroke. He states, yes and
yes. Heat deaths have doubled in recent decades. This is an issue for all who
work in hot environments. Heat + a core temp of over or equal to 104 degrees F,
combined with a high index of suspicion = Heat Stroke. There is a 30-minute
target for dramatic reduction in core temperature. Cold packs at pulse points
do not provide enough cooling. Cold packs do not even get cold enough to
provide the level of cooling needed. Use cold water immersion. The sooner the
cooling starts the better. It should not wait till arrival at the hospital.
Cool first, transport second. Adapt a body bag to hold ice and water for this
purpose. You can also use a tarp as a taco. It is now their protocol, and it
has been working well. Twenty patients treated so far. Being used in DFW and
San Antonio.
Lawner - Trauma Arrest – Re-analyze our Management of
Traumatic Arrest: NAEMSP and ACS have a TOHCA algorithm. CPR is not as
important as the proven life-saving interventions. If you want to do
compressions, do so, but do not let it get in the way of what might work.
Giving blood and controlling the airway have proven benefits toward outcomes.
There is zero benefit that compressing a heart with no blood in it does
anything positive, in fact it may hinder residual cardiac perfusion. Things
that matter when the conditions are present: Manage the airway, bind the
pelvis, decompress the chest, perform pericardiocentesis, and stop
exsanguination.
Miramontes – Red or Dead? On-scene Trauma Triage: Some
thoughts on atypical scene management. Shows START Triage algorithm.
Complicated. Shows SALT algorithm. If flash bangs or explosions, SALT is
useless as no one can hear you to follow you. If you are shot or stabbed in the
box, you do not need a tag, you need an operating room. Stop bleeding, get an
airway (simple), and move them to the truck. Movement is the most important
component. Get the cluck to the truck. You need engine companies for the sole
purpose of helping move patients to trucks. Abandon triage tags. What about
lightning strike MCI? Three people down. Always use reverse triage with
lightning. The dead are treated first. Again, you need a lot of people to move
the patients. The dead are the most salvageable in this case. Case study from
Walmart on July 23, 2017. Walmart assisted green and yellow patients with water
and support. Declare deaths and shield the dead from other responders to reduce
PTSD. June 27, 2022 Quintana Road case study with multiple patients and bodies
in back of a semi trailer. Officer did a Red or Dead method as the semi was
full of people. Police cars can clog MCI scenes. Have someone move them to
create entry and egress corridors. Designed their own triage algorithm. Hide
the dead from public and responder view. Size up the scene. Go through command.
Do airway and required stuff that works and get the cluck to the truck. Have a
plan for fatality management.
Calhoun – Why We Need to re-analyze the use of chest seals:
Stop buying them. They do not do what we have been told they do. They only trap
air inside. The only thing they may do is help reinflate the lung if there is
spontaneous breathing. Most of the time this is not needed. These waste funds
and time. Never use on a patient receiving PPV.
Sandoval/Feldman – Are Current Call-Takers Questions and 911
Deployment Codes Correct? How accurate is medical incident dispatch? Using card
12 (seizures) for the analysis. Looked at frequency of Midazolam utilization by
the ambulance. Most calls were delta responses. 34 were actually arrests and
some of the arrests were dispatched as Alpha through Charlie calls. Findings:
Two questions on the card predicted acuity. Those were history of seizures and
history of brain cancer. This can be done for any card/protocol. Response case
can be correlated to EPCR and then hospital outcome if needed. In EMD, no
perfect precision is possible. “EMD is a massive public health screening
exercise.” The impact is significantly positive, but not perfect. EMD catches
far more than it misses. Maybe we compare the standard to the protocol to
assure the response correlates to the protocol. Doing this will cause some
things to move. For example, is a fall still on the floor an alpha response? Look
for things that are under prioritized by correlating with the EPCR. Use
performance improvement cycles.
So those are all of my notes from Eagle’s 2025. I hope that
you can utilize this information to stimulate advancement and improvement within
your EMS operations. I cannot promote this annual meeting enough. Please
consider attending. They keep the prices low so that as many people that can
attend get the opportunity.